Introduction:
Slipped Capital Femoral Epiphysis (SCFE) is a relatively rare but potentially serious hip disorder that mainly affects adolescents during their growth spurts. This condition occurs when the ball at the top of the thigh bone (femur) slips off the neck of the bone at the hip joint. Understanding SCFE is crucial for early detection and treatment to prevent long-term complications. In this article, we delve into the causes, symptoms, diagnosis, and treatment options for SCFE.
What Causes SCFE?
The exact cause of SCFE is not fully understood, but it is believed to be related to a combination of factors, including:
Growth spurts: SCFE often occurs during periods of rapid growth, typically in pre-adolescents and adolescents. The growth plate at the top of the femur is weaker during these growth spurts, making it more susceptible to slipping.
Obesity: Excess weight puts added pressure on the growth plate, increasing the risk of it slipping. Obese children are more likely to develop SCFE compared to those of normal weight.
Hormonal changes: Hormonal changes during puberty may also contribute to the weakening of the growth plate, making it more prone to slipping.
Genetics: There may be a genetic predisposition to SCFE, as it tends to run in families.
SCFE can present with various symptoms, which may include:
Hip or knee pain: Persistent pain in the hip, groin, thigh, or knee, particularly during physical activity, is a common symptom of SCFE.
Limping: A noticeable limp or inability to bear weight on the affected leg may occur due to pain and instability in the hip joint.
Limited range of motion: Reduced flexibility and range of motion in the hip joint may be observed, making it difficult to perform certain movements.
Outward rotation of the leg: The affected leg may appear to turn outward due to the displacement of the femoral head.
Diagnosis of SCFE:
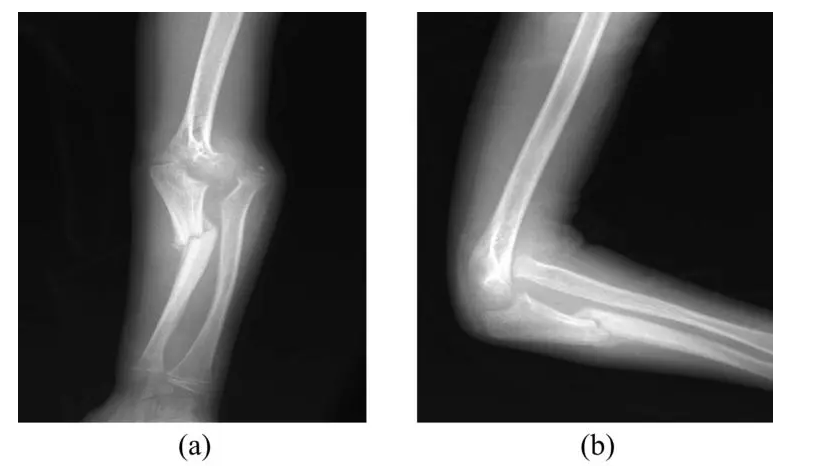
Diagnosing SCFE typically involves a combination of medical history review, physical examination, and imaging tests. The healthcare provider will inquire about the child's symptoms and perform a physical examination to assess the range of motion and stability of the hip joint.
Imaging tests are essential for confirming the diagnosis and determining the severity of the condition. X-rays are commonly used to visualize the position of the femoral head relative to the femoral neck. In SCFE, characteristic findings on x-rays include a slippage of the femoral head in relation to the neck, often described as a "ice cream slipping off a cone" appearance.
In some cases, additional imaging studies such as MRI or CT scans may be ordered to obtain more detailed images of the hip joint and surrounding structures.
Treatment Options for SCFE:
The primary goals of treatment for SCFE are to stabilize the hip joint, relieve symptoms, and prevent further slippage. The treatment approach may vary depending on the severity of the condition and the child's age and overall health. Common treatment options include:
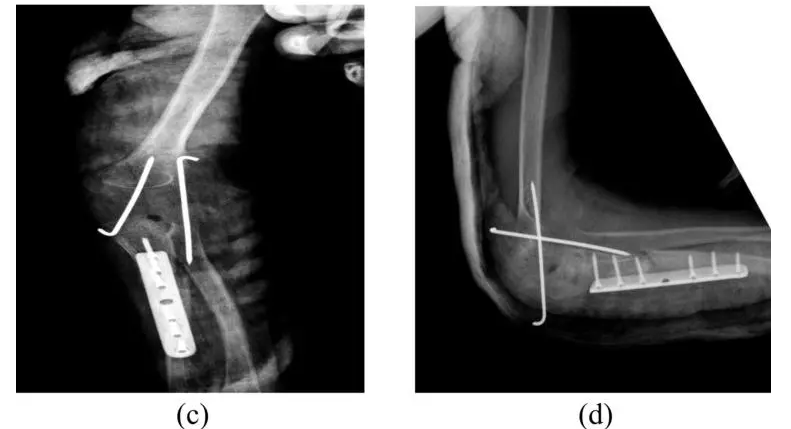
Surgical intervention: In most cases of SCFE, surgery is necessary to stabilize the hip joint and prevent further slippage. The two main surgical procedures used to treat SCFE are:
a. In Situ Fixation: This involves inserting screws or pins into the femoral head and neck to hold them in place and prevent further slippage.
b. Realignment Osteotomy: In severe cases or when the slip is chronic, a realignment osteotomy may be performed to reposition the femoral head and neck into the correct alignment.
Non-surgical management: In some mild cases of SCFE, non-surgical measures such as rest, activity modification, and physical therapy may be recommended to alleviate symptoms and prevent worsening of the condition. However, close monitoring is essential to detect any progression of the slip.
Post-operative Care and Rehabilitation:
Following surgery, a period of immobilization and restricted weight-bearing may be necessary to allow the hip joint to heal properly. Physical therapy is an integral part of rehabilitation to improve strength, flexibility, and mobility of the hip joint. The rehabilitation process is tailored to each individual's needs and may continue for several months to achieve optimal recovery.
Long-term Outlook:
With prompt diagnosis and appropriate treatment, most children with SCFE can expect favorable outcomes and return to normal activities. However, untreated or poorly managed SCFE can lead to serious complications such as hip joint deformity, osteoarthritis, and chronic pain later in life. Regular follow-up appointments and monitoring are essential to detect any signs of recurrence or complications early on.
Conclusion:
Slipped Capital Femoral Epiphysis (SCFE) is a potentially debilitating hip disorder that primarily affects adolescents during their growth spurts. Early recognition of symptoms and timely intervention are crucial for preventing long-term complications and ensuring optimal outcomes. By understanding the causes, symptoms, and treatment options for SCFE, healthcare providers, parents, and caregivers can work together to provide the best possible care for children affected by this condition.